Missing Teeth? Find Your Smile Again.
Acute Tooth Pain: What to Expect at the Dentist, Immediate Relief, and a 14-Day Healing Roadmap
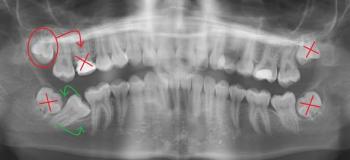
Severity:
Teeth Problems:
Quick visual impression
I can’t give a definitive diagnosis from photos alone, but the image shows a large existing restoration (amalgam or metal) on a lower molar with surrounding gum redness. The appearance and your description of “horrible, stinging pain” suggest one of the following is likely:
-
failing/restored tooth with recurrent decay reaching the pulp,
-
pulpitis (inflamed nerve) possibly progressing to irreversible pulpitis, or
-
an abscess forming beneath the tooth (less visible externally early on).
A broken or leaking filling can let bacteria into the tooth and cause sharp, severe pain.
What the dentist will likely do at your visit
-
Triage / pain control — ask about symptoms, meds you’ve tried, and medical history (bring Medicaid card).
-
Clinical exam — look, probe the tooth and gums, check for swelling, and test biting sensitivity.
-
X-ray (periapical or bitewing) — to assess decay depth, root status, and any abscess.
-
Initial treatments depending on findings:
-
If reversible pulpitis / minor decay: remove decay and place a new filling.
-
If irreversible pulpitis or pulp necrosis: the dentist will recommend root canal therapy (RCT) to save the tooth — often same-week referral or performed at the clinic.
-
If the tooth is non-restorable or the patient prefers: extraction may be performed.
-
If there is active infection with swelling: drainage and/or a course of antibiotics may be prescribed (antibiotics alone won’t fix a dead nerve — RCT or extraction still needed).
-
Temporary measures: a sedative dressing, temporary filling, or analgesic pack to control pain until definitive care.
-
-
Follow-up plan — permanent restoration (crown) after RCT if the tooth is saved, or healing instructions after extraction.
What to expect with Medicaid
-
Many clinics and community dental clinics accept Medicaid for urgent care, RCT, extractions, and restorations — coverage varies by state.
-
Call ahead, explain you have severe pain and Medicaid — ask for same-day/urgent slot. Many offices hold emergency appointments for painful patients.
-
If you have trouble finding a provider, consider community health centers, dental schools, or local clinics listed on your state Medicaid site. (You can also try your clinic link: https://cebudentalimplants.com/map-dental-clinic — though that’s Philippines-focused, so for local U.S. care check state Medicaid resources.)
Immediate (safe) steps you can take right now for relief
(Do these until you can see a dentist.)
-
Pain relief meds
-
Ibuprofen 200–400 mg every 4–6 hours as needed (do not exceed label max / consider medical contraindications).
-
Acetaminophen (paracetamol) 500–1000 mg every 4–6 hours as needed (stay within daily max).
-
If one alone isn’t enough, alternating ibuprofen and acetaminophen can be effective — but don’t exceed recommended doses. If you’re on blood thinners, have liver/kidney disease, or other concerns, check with a provider first.
-
-
Warm saline rinse (1 teaspoon salt in 8 oz warm water) gently after meals — do NOT vigorously swish if you suspect an open socket or fresh extraction.
-
Cold compress outside the cheek for 15 minutes on / 15 off to reduce throbbing swelling.
-
Avoid chewing on that side and avoid very hot or cold foods if they cause sharp pain.
-
Topical relief (optional & temporary): over-the-counter benzocaine gel or clove oil dabbed to the painful area can help short-term — use small amounts and follow product directions; avoid if allergic.
-
Elevate head when resting — reduces blood flow to the head and sometimes eases throbbing.
Note: If you have fever, spreading swelling, trouble breathing/swallowing, or rapidly worsening symptoms — go to ER or urgent dental care immediately.
14-day healing expectation (typical scenarios)
-
If treated promptly with RCT or extraction + proper care: pain should drop significantly within 24–72 hours. By 7–14 days, swelling and most discomfort should be gone and the soft tissues mostly healed. Final restorations (crowns) may be placed after RCT once tooth is stable.
-
If only temporary measures are used: pain may persist or recur until the tooth is definitively treated.
-
If left untreated: pain and infection can worsen, potentially forming a dental abscess, spreading to adjacent teeth or soft tissues, and requiring more complex treatment (longer antibiotics, drainage, or surgery). Healing will not occur without dental intervention if the pulp is necrotic or abscessed.
What can “scale up” if you delay care
-
Worsening infection → swelling, bone involvement (rare osteomyelitis), or spread to facial/neck spaces (medical emergency).
-
Loss of the tooth or need for extraction instead of a tooth-saving root canal.
-
More costly and extensive treatment later (implant, bridge, or more complex surgery).
-
Systemic risk in immunocompromised patients (sepsis risk is low but nonzero).
Practical next steps (action list)
-
Call an urgent dental clinic now and ask for an emergency appointment — say “severe tooth pain, swelling? I have Medicaid.”
-
Bring your Medicaid info, photo(s), and any medications you’re taking.
-
Use pain-control steps above until you’re seen.
-
If the clinic suggests antibiotics or pain meds, follow instructions exactly and ask about follow-up RCT or extraction scheduling.