We Bring Back the Sparkle in Your Smile.
The Painless Puncture: How Microneedles are Set to Revolutionize Dentistry
Language :
Topics:
For generations, the core tools of dentistry have been, by necessity, invasive. The drill, the scaler, and the syringe needle, while effective, are instruments that trigger deep-seated anxiety in patients. But what if we could deliver treatment not with a roaring drill or a painful jab, but with a silent, painless, and dissolvable patch?
This is the promise of microneedles—a technology poised to usher in a new era of minimally invasive, highly precise dental care.
What Are Microneedles? The Science of the Tiny
Imagine an array of microscopic needles, so small that 100 of them could fit on the tip of a single traditional dental needle. These are microneedles.
-
Composition: They are typically fabricated from biodegradable polymers like hyaluronic acid, polylactic-co-glycolic acid (PLGA), or silk. These materials are strong enough to penetrate tissue but then safely dissolve within it.
-
The Genius of the Design: Their length is meticulously engineered (typically 50-900 micrometers) to be:
-
Long enough to painlessly breach the non-sensitive enamel surface or to deliver drugs through the gum tissue to the area around a tooth's root.
-
Short enough to avoid contacting the underlying nerve-rich dentin or pulp, thereby causing no significant pain or bleeding.
-
This creates a direct, controlled pathway for therapeutic agents, bypassing the main barriers to effective treatment.
The Discovery: From Transdermal Patches to Oral Mucosae
The story of microneedles did not begin in the dental chair. They were first conceptualized and developed in the 1990s for transdermal drug delivery, as a painless alternative to hypodermic needles for vaccines and insulin.
The "Eureka!" moment for dentistry came when researchers realized that the oral mucosa (the lining of the mouth) and the tooth enamel presented unique, ideal environments for this technology. The oral mucosa is highly permeable, and the enamel, while the hardest substance in the human body, has a non-living, non-sensitive surface layer that is perfect for superficial micro-perforations. The adaptation from skin to mouth was a logical, yet brilliant, leap.
The AI Accelerator: Supercharging Microneedle Development
The journey from a lab concept to a clinical product is long and fraught with challenges. This is where Artificial Intelligence acts as a powerful catalyst, accelerating every step.
-
AI in Material Discovery: AI algorithms can model and simulate millions of polymer combinations to predict their properties: How fast will they dissolve? How much drug can they hold? How strong are they? This slashes years off the traditional "trial and error" material science phase.
-
Precision Design and Optimization: Using generative design AI, researchers can input desired outcomes (e.g., "maximize drug payload while ensuring dissolution within 30 minutes"). The AI then generates thousands of optimal microneedle designs—shapes, lengths, and array patterns—that a human might never conceive of.
-
Accelerating Clinical Trials: AI can analyze vast datasets from early-stage trials to identify which patient profiles respond best to the treatment, predict potential side effects, and optimize dosing regimens. This makes clinical trials faster, cheaper, and more effective.
The Latest News: From Lab to Clinic - Real-World Applications
The research is rapidly moving beyond theory. Here are the most exciting and recent developments:
-
The End of the Drill and Fill? Researchers at the University of Washington and others are developing microneedle patches for remineralizing early cavities. The needles create micro-channels in the enamel, allowing a high concentration of calcium, phosphate, and fluoride to seep deep into the lesion, effectively reversing the decay without any drilling.
-
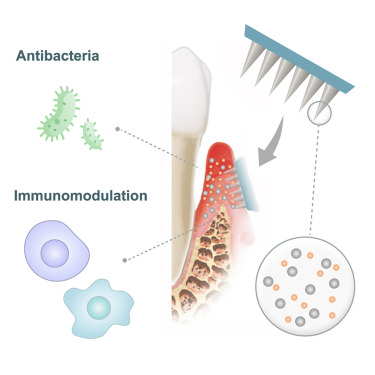
Targeted Periodontal Therapy: A major challenge in treating gum disease is getting antibiotics deep into the periodontal pocket. Studies now show that a microneedle patch can be pressed against the gum to deliver a high dose of antimicrobials directly to the site of infection, vastly improving efficacy over traditional rinses or oral antibiotics.
-
Pain Management Revolution: Imagine a small patch applied to the gum before an injection, delivering a local anesthetic painlessly through microneedles. This could make the dental needle itself obsolete for many procedures, eliminating the number one fear of patients.
-
Desensitizing Teeth: For patients with sensitive teeth, a microneedle patch could deliver desensitizing agents like potassium nitrate directly into the dentinal tubules, providing long-lasting relief.
The Future is Minimal
The integration of microneedles represents a fundamental shift from a "macro" to a "micro" approach in dentistry. It's a move away from removal and restoration and towards precision biologic management.
In the next decade, a visit to the dentist for an early cavity might not involve a drill, but the application of a small, silent patch. Treatment for gum disease may be a targeted, painless application rather than invasive surgery. The potential to improve patient comfort, enhance treatment outcomes, and make dental care truly preventative is immense.
The age of the painless puncture is dawning, and it will change everything we know about going to the dentist.












